|
A functionally unstable spine may be the cause of a person's back pain. It is a painful disorder thought to result from a loss of the spine’s ability to maintain appropriate mechanical stiffness throughout it's NORMAL range of movements. In biomechanical terms, spinal stiffness refers to the spine’s ability to prevent unwanted movement or buckling. People often think of stiffness as a bad thing. It isn't always. When a muscle contracts, it creates both force and stiffness. Spinal stiffness is necessary to perform basic daily movements. With minimal amount of force, muscles around the spine act as guy wires, a tensioned cable designed to add stability to a free-standing structure.
It is important to note that a functionally unstable spine is not synonymous with hypermobility or radiographic instability. Hypermobility and radiographic instability is where spinal joint motion is excessive BEYOND normal joint movement. This is typically demonstrated on appropriate imaging. Some indicators that a functionally unstable spine may be the cause of a person's back pain often include:
40-60% of typical back pain patients experience recurrence or low level chronic symptoms, but a pattern of sudden flare ups caused by minimal loading events may be linked in this instability phenomena. The theory behind this is that poor stability increases the risk of a “spinal buckling” under minimal weight, often just bodyweight movements, and triggers episodes. This accumulative repetitive buckling makes it difficult for the patient to truly feel a healing of their back pain. The safest and most effective conservative treatment for patients with a functionally unstable spine is through an effective spine stabilization exercise routine. Stabilization exercises are designed to improve spinal stability, relieve pain and increase movement performance. A large number of muscles cross the spine, and all contribute to the modulation of lumbar stability and movement to some extent. Multiple imaging studies have demonstrated muscle atrophy in patients with chronic back pain. A stabilization exercise routine is designed to target these areas of muscle atrophy to improve strength and reduce muscle fatigue over time. Some of the muscles that are most commonly weakened and atrophied in patients with a functionally unstable spine are:
Most people are surprised to learn that the diaphragm, which is mainly involved in breathing, is a key muscle in creating spinal stability. As the roof of the cylinder of muscles that surround the spine and assist with stability, the diaphragm is a major contributor to intraabdominal pressure and therefore lumbar stability. The diaphragm contributes to this spinal stiffness before the initiation of large limb movements to assist with spinal stability and greater strength of the arms or legs. Some of the most effective stabilization exercises studied include:
Once these exercises are mastered, a person suffering from a functionally unstable spine can gradually progress to various bodyweight loading strategies that would ordinarily be seen a training weight training environment. This type of training of the spine will carry over into the performance of functional activities, daily living activities, and work ultimately resulting in reduced episodes of functionally unstable back pain. If you feel your back pain is the result of a functionally unstable spine, please click the link below to request an appointment!
0 Comments
Incorrect use of a proper back pack can be just as damaging as using an improper back pack. Our growing children use their back packs for many years. Repetitive loading of heavy back packs combined with poor ergonomics can be a source of dysfunction in their body and can lead to chronic back and shoulder pain. Smart choices now are important to your child's health long after their school days are gone.
Signs that your child's back pack is inappropriate for them or that they are wearing the pack incorrectly include:
When purchasing a new back pack one should look for:
Maintain regular adjustments with your chiropractor to detect and correct spinal problems before they cause pain and dysfunction in your growing child. Additional tips for proper back pack ergonomics:
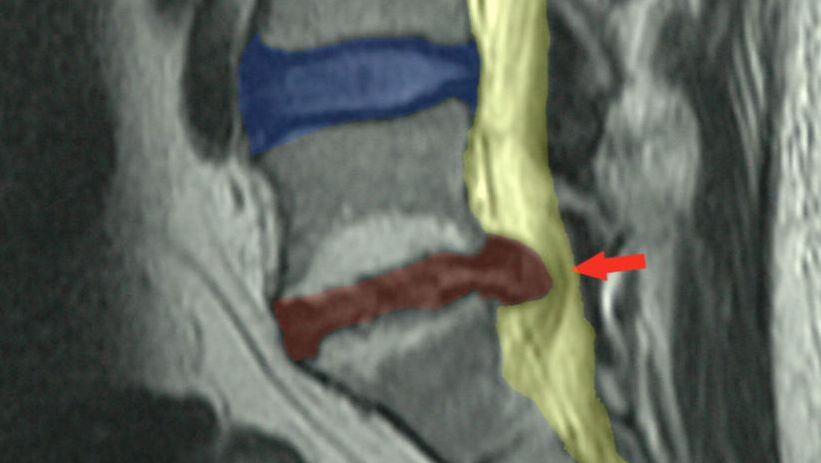
When a patient is diagnosed with a lumbar disc herniation, what is the best treatment?
Best Answer: Both conservative and surgical options are backed by research. Though the ultimate decision of which route to choose should be made by the patient based on their individual goals and needs after an honest discussion with their surgeon. Now let's talk! Lumbar disc herniations are a very common condition affecting the spine of young and middle-aged folks. The incidence of lumbar disc herniations within certain populations has been estimated to be greater than 50% though often the disc herniations is asymptomatic, meaning without symptoms. A disc “injury” quite often happens in the absence of any pain and you don’t even know about it. Medicare estimates that spending on lumbar discectomy procedure, a surgery to remove disc material, exceeds $300 million annually. Back pain related disorders may or may not always be the result of a disc herniation but are a common cause of disability nonetheless. The American health care system spends over $1 billion annually to address back pain conditions. The structure of the disc is composed of circular, basket woven-like annular fibers made of collagen, proteoglycans, and a variety of regenerative cells that surround a gel like structure called the nucleus pulposus. The disc serves to dissipate forces exerted on the spine as well as give space between the vertebra above and below the disc so the nerves have room to exit the spine. As we age, the disc tends to lose water content and height. This loss of hydration and disc collapse can increase strain on the annular fibers which may lead to bulging, a protrusion or extrusion of disc material that would be seen as a herniation. The joint made up between the two vertebral bones and disc is called the intervertebral joint. It is classified as a fibrocartilage joint and can also be referred to as a symphysis joint, similar to the pubic symphysis of the pelvis. If you know anything about symphysis joints, you know that they are EXTREMELY STRONG and they certainly don't slip out of place, giving the impression that discs are inherently weak. It takes about 740lbs of force to compress the disc height 1mm in young subjects and 460lbs of force to compress the disc height 1mm in older subjects. End story is that discs are VERY strong. With all that said, back pain may still occur due to disc bulging without pressure on the spinal canal or nerve roots. However back pain with radiculopathy can occur when pressure or irritation of the extruded disc material contacts the thecal sac or lumbar nerve roots. The pain commonly felt with radiculopathy can be felt as electrical, shooting, pins and needles, numbness, tingling, or weakness into the leg. Often patients will experience this as "Sciatica". Sciatica is a description of any of the symptoms above felt in the leg as a result of pressure or irritation of the specific nerve roots levels of L4, L5, or S1. The good news is that 90% of patients with lumbar disc herniations will improve without substantial medical intervention like surgery. Too many people think that once you have a disc herniation (or disc bulge), that you’ve got it for life. Discs have the ability to heal. A patient should not be fearsome of low back pain, even if pain is caused by a disc injury. Regarding treatment, the research supports both conservative management and surgical intervention as viable options for the treatment of lumbar disc herniation even when radiculopathy is present. Surgical intervention may result in faster relief of symptoms and earlier return to function, although long-term results studies show similar outcomes regardless of type of management. It should be noted that contrary to popular belief of some including surgeons, the size of a lumbar disc herniation does not predict outcomes or the need for surgery. Research indicates from many studies, multiple medical association position statements, and my own clinical experience treating these disorders validates this notion. This is consistent with findings from a 2010 study which found that even massive disc herniations can successfully be treated conservatively. In fact, on several occasions patients with nearly complete spinal canal narrowing were successfully managed without surgery, some as great as 85.1%. Literature suggests that less than 10% of disc herniation cases ultimately require surgery. The typical patient with lumbar disc related pain will often present to their primary care physician first. However research supports chiropractors being a great first contact for these patients. In fact, medical costs may significantly be reduced when a patient visits a chiropractor first. Initial management of these disorders should include regular movement within a patient's tolerance, exercise guidance, manipulation of the spine, proper nutrition and supplementation, and adequate sleep. A patient should not be told to completely rest. Many of these patients are able to continue lifting. In most instances, radicular symptoms will go away within six weeks. Patients with symptoms that persist beyond six weeks will often be referred for advanced imaging like magnetic resonance imaging (MRI) in order to identify the area of disc pathology and to determine if they are also candidates for more invasive treatments like injection or surgery. If you are suffering from back pain, please click the link below to request an appointment! Thirty-one million Americans have low back pain at any given time.1 One half of all working Americans admit to having back symptoms each year. 2 One third of all Americans over age 18 had a back problem in the past five years severe enough for them to seek professional help. 3 And the cost of this care is estimated to be a staggering $50 Billion yearly–and that’s just for the more easily identified costs!4
These are just some of the astounding facts about Americans and their miserable backs! Is there any wonder why some experts estimate that as many as 80% of all of us will experience a back problem at some time in our lives?5 Because back problems are this common it’s probably going to happen to you too! Shouldn’t you find out what to do about it before it happens rather than after? Why wait until you’re hurting to learn about your treatment options? When you’re hurting you may not give this important decision the time and attention it needs to make the best choice. Here are the facts about manipulation as a treatment for back problems: Manipulation is one of several established forms of treatment used for back problems. Used primarily by Doctors of Chiropractic (DCs) for the last century, manipulation has been largely ignored by most others in the health care community until recently. Now, with today’s growing emphasis on treatment and cost effectiveness, manipulation is receiving much more widespread attention. In fact, after an extensive study of all currently available care for low back problems, the Agency for Health Care Policy and Research–a federal government research organization–recommended that low back pain suffers choose the most conservative care first. And it recommended spinal manipulation as the ONLY safe and effective, DRUGLESS form of initial professional treatment for acute low back problems in adults!6 Chiropractic manipulation, also frequently called the chiropractic adjustment, is the form of manipulation that has been most extensively used by Americans for the last one hundred years.7 Satisfied chiropractic patients already know that DCs are uniquely trained and experienced in diagnosing back problems and are the doctors most skilled in using manipulation for the treatment of back pain and related disorders.8 As a public service, the American Chiropractic Association (ACA) urges you to make an informed choice about your back care. To learn more about the federal government’s recommendations and how chiropractic manipulation may help you, contact a Doctor of Chiropractic in your area. References:1. Jensen M, Brant-Zawadzki M, Obuchowski N, et al. Magnetic Resonance Imaging of the Lumbar Spine in People Without Back Pain. N Engl J Med 1994; 331: 69-116. 2. Vallfors B. Acute, Subacute and Chronic Low Back Pain: Clinical Symptoms, Absenteeism and Working Environment. Scan J Rehab Med Suppl 1985; 11: 1-98. 3. Finding from a national study conducted for the American Chiropractic Association. Risher P. Americans’ Perception of Practitioners and Treatments for Back Problems. Louis Harris and Associates, Inc. New York: August, 1994. 4.This total represents only the more readily identifiable costs for medical care, workers compensation payments and time lost from work. It does not include costs associated with lost personal income due to acquired physical limitation resulting from a back problem and lost employer productivity due to employee medical absence. In Project Briefs: Back Pain Patient Outcomes Assessment Team (BOAT). In MEDTEP Update, Vol. 1 Issue 1, Agency for Health Care Policy and Research, Rockville, MD, Summer 1994. 5.In Vallfors B, previously cited. 6.Bigos S, Bowyer O, Braen G, et al. Acute Low Back Problems in Adults. Clinical Practice Guideline No. 14. AHCPR Publication No. 95-0642. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services, December, 1994. 7.The RAND Corporation reported from its analysis of spinal manipulation research literature that 94% of all spinal manipulation is performed by chiropractors, 4% by osteopaths, and the remainder by medical doctors. Did you just sprain your ankle? I did recently. It hurts! Ankle sprains occur so often that sometimes it can be easy to overlook helpful treatment strategies to accelerate the healing because, well, they will heal on their own, right?
Ankle sprains are the most common lower extremity injury in sport. The most common is an inversion sprain where the foot rolls under the inside portion of the ankle. There are eversion sprains and diastasis (aka "high ankle") sprains, but these are less common. Now more than ever it seems the world wants effective means by which to naturally boost the immune system. We've already learned a lot about what strengthen our immunity before this pandemic and even more afterwards. What we know is that functional impairment of antigen-specific T cells is a hallmark of chronic infections and viral disease. There are many considerations for boosting immunity and T cell function. Supplements most notable for this are:
Want more tips and tricks on keeping your body healthy and strong? Hit us up at Gaitway Chiropractic @ Spokane Wellness in Spokane, Wa. 509-466-1366 References:
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. What conservative treatments for pain do Chiropractors and physical therapist typically use?12/18/2020 Effective conservative treatments for musculoskeletal related pain that you will most often find in the chiropractic or physical therapy clinic include:
Of course, there exists other conservative treatment options like nutritional needs analysis, topical analgesics, acupuncture, brain based therapy, hypobaric oxygen therapy, etc. However, the list above is what most often what a Chiropractor or physical therapist might recommend to you. Before you decide which treatment or combination of treatments you decide to go with, it is important for you to be an equal team member in the decision making process of your own health. Want tips and tricks on getting rid of headaches, back pain, neck pain, shoulder pain, hip pain, knee pain for good? Hit us up at Gaitway Chiropractic at Spokane Wellness in Spokane, Wa. 509-466-1366 Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Deep referred pain is also called "scleratogenous" referred pain and is far more likely a cause of symptoms referring down a patient's arms or legs than is a true nerve root or "radicular" problem. We also call deep referred pain "somatic referred pain" where the "soma" or body tissues like muscles, bone, joint, ligaments, skin and fascia. Once a trained clinician in the area of pain has ruled out central and peripheral nerve damage, their consideration of a patient's pain source causing referral should be that of joints, ligaments, or muscles. This is the most common scenario. The cause of this type of referred pain comes from our understanding of a patient's modulation of pain perception. There are several proposed theories for referred pain including:
Examples of a patient's deep referred, "somatic" or "scleratogenous", referred pain that is most commonly seen with spinal related complaints could be from things like:
Though describing the concept of deep referred pain as above may make it sound simple and easy to comprehend, the truth is that deep referred pain can overlap considerably with other clinical pain presentations and differentiation may be difficult. A way to remember "scleratogenous" pain is that it may be:
Want tips and tricks on getting rid of deep referred pain for good? Request an appointment now. Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The research linking Vitamin D deficiency and the effects of COVID-19 along with the severity of COVID-19 outcomes and treatment with vitamin D is mounting up.
We told you about a pilot study a while back that was released in August 2020 to assess the clinical effectiveness of treatment of patients hospitalized for COVID-19 with calcifediol (25-hydroxyvitamin D3). The highlights of this study indicated that the vitamin D endocrine system may have a variety of actions on cells and tissues involved in COVID-19 progression and that the administration of calcifediol or 25-hydroxyvitamin D to hospitalized COVID-19 patients significantly reduced their need for Intensive Care United admission. (Castillo et al 2020). Vitamin D seems to be able to reduce severity of the disease. But wait, there's more. Researchers in Spain found that 82.2% of COVID-19 patients tested were found to be deficient in vitamin D. (Hernández et al 2020) Aside from the impact of insulin resistance on the severity of COVID-19 outcomes, Vitamin D deficiency is emerging as a primary risk factor for the severity of COVID-19 infections. It would be foolish to not consider assessing one's current serum 25-hydroxyvitamin D (25OHD) and determining the best supplementation to address increasing that level over time. For instance, for an individual weighing 185 lbs that was categorized at a high risk for viral infection with low vitamin D levels in the blood measuring at 10 ng/ml and wished to increase their amount to a high vitamin D level of 60 ng/ml in order to lower their risk of infection, that person would need a supplementation amount of: 10000 IU* per day (more than their current intake) to be sufficient to achieve the recommended target serum level of 60 ng/ml. *Values rounded to the nearest 1000 IU Vitamin D plays a significant role in our health. It can reduce the survival and replication of viruses, reduce cellular inflammation, maintain vascular integrity by effecting vascular inflammation and clotting factors, reduce blood pressure by it's role in the conversion of angiotensin-converting enzyme 2, lower cancer risk, improve bone and connective tissue healing, decrease risk of autoimmune disease, and more. To optimize vitamin D absorption and utilization, be sure to take your vitamin D with vitamin K2 and magnesium. A person supplementing Vitamin D for the hope to raise serum blood levels should retest their serum 25-hydroxyvitamin D (25OHD) every three to four months. References: Castillo M.E., Entrenas Costa L.M., Vaquero Barrios J.M., Alcalá Díaz J.F., Miranda J.L., Bouillon R., Quesada Gomez J.M. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 2020;203:105751. doi: 10.1016/j.jsbmb.2020.105751 José L Hernández, Daniel Nan, Marta Fernandez-Ayala, Mayte García-Unzueta, Miguel A Hernández-Hernández, Marcos López-Hoyos, Pedro Muñoz Cacho, José M Olmos, Manuel Gutiérrez-Cuadra, Juan J Ruiz-Cubillán, Javier Crespo, Víctor M Martínez-Taboada, Vitamin D Status in Hospitalized Patients With SARS-CoV-2 Infection, The Journal of Clinical Endocrinology & Metabolism, , dgaa733, https://doi.org/10.1210/clinem/dgaa733 With COVID-19 still on the table and the upcoming seasonal occurrences of cold and flu, targeting the immune system and improving one's overall wellness is critical. The right vitality and nutrition plan during this time has the potential to help decrease the frequency, severity, or duration of cold and flu symptoms.
We can decrease this risk with:
This is even more important for high-risk populations, such as the elderly, those who are overweight, those with diabetes and other comorbidities causing compromised immune systems. Want tips and tricks on keeping your body strong during this upcoming cold and flu season? Are you sick now and wish you were more prepared to fight off the cold or flu virus so you can more quickly return to what you enjoy? Then follow along with this protocol developed using only quality evidence. The following protocol and ingredients below are a reflection of what current research findings show support for when trying to prevent or treat the immune system affecting by cold and flu viruses. Vitamin C Adults: 1 g daily as an ongoing maintenance dose3,4, or 3 to 4 g daily at the onset of symptoms and for the duration of illness2,4 Children: 1 to 2 g daily as an ongoing maintenance dose4,2
Zinc 75-100 mg of elemental zinc as zinc acetate or zinc gluconate lozenges, once per day, within 24 hours of the onset of common cold symptoms, minimum 1 to 2 weeks cold15,16,17,18,19
Probiotics Probiotics may reduce the incidence of colds with minor effects on prevention, as well as improve influenza vaccination efficacy for A/H1N1, A/H3N2, and B strains, but is dependent on strain and population.24,25,26 Pediatric: Common Cold
Common Cold
Echinacea purpurea Prevention: 0.9 mL, three times per day (equivalent to 2400 mg of extract), minimum 4 months9 Acute: Up to 4.5 mL liquid extract (equivalent to 4000 mg), once per day at the first stage of cold development9
American ginseng (Panax quinquefolius) 400 mg, once per day, minimum 8-16 weeks in healthy adults as a preventative measure5,6,7
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Did you know we have a supplement protocol designed with the above cold and flu support topic discussed above. Check it out! https://us.fullscript.com/protocols/spokane-wellness-immune-health-cold-and-flu-support References 1https://www.ncbi.nlm.nih.gov/pubmed/30069463 2https://www.ncbi.nlm.nih.gov/pubmed/23440782 3https://www.ncbi.nlm.nih.gov/pubmed/19592479 4https://www.ncbi.nlm.nih.gov/pubmed/16247099 5https://www.ncbi.nlm.nih.gov/pubmed/16566675 6https://www.ncbi.nlm.nih.gov/pubmed/14687309/ 7https://www.ncbi.nlm.nih.gov/pubmed/23024696 8https://www.ncbi.nlm.nih.gov/pubmed/24554461 9https://www.ncbi.nlm.nih.gov/pubmed/16678640 10https://www.ncbi.nlm.nih.gov/pubmed/17597571 11https://www.ncbi.nlm.nih.gov/pubmed/14748902 12https://www.ncbi.nlm.nih.gov/pubmed/16177972 13https://www.ncbi.nlm.nih.gov/pubmed/28515951 14https://www.ncbi.nlm.nih.gov/pubmed/22566526 15https://www.ncbi.nlm.nih.gov/pubmed/27378206 16https://www.ncbi.nlm.nih.gov/pubmed/23775705 17https://www.ncbi.nlm.nih.gov/pubmed/28480298 18https://www.ncbi.nlm.nih.gov/pubmed/25888289 19https://www.ncbi.nlm.nih.gov/pubmed/18279051 20https://www.ncbi.nlm.nih.gov/pubmed/17344507 21https://www.ncbi.nlm.nih.gov/pubmed/23372900 22https://www.ncbi.nlm.nih.gov/pubmed/29416317 23https://www.ncbi.nlm.nih.gov/pubmed/29077061 24https://www.ncbi.nlm.nih.gov/pubmed/19651563 25https://www.ncbi.nlm.nih.gov/pubmed/20803023 26https://www.ncbi.nlm.nih.gov/pubmed/17352961 27https://www.ncbi.nlm.nih.gov/pubmed/21285968 28https://www.ncbi.nlm.nih.gov/pubmed/20180695 29https://www.ncbi.nlm.nih.gov/pubmed/18335698 |
Dr. Jared Wilson, DC, MSDr. Jared Wilson blogs about chiropractic health and other relevant health news. He is an expert in musculoskeletal injuries and functional rehab. He holds a Chiropractic Doctorate degree and a Masters degree in Exercise and Sports Science. Archives
August 2023
Categories |





 RSS Feed
RSS Feed